This blog post is to help you prepare for the ‘what if’ scenario if you need an assisted delivery for the birth of your baby.
An assisted delivery means when a doctor uses an instrument such as forceps or ventouse cup (sometimes called a Kiwi cup) to deliver your baby’s head. Around one in eight women deliver their baby in this way in the UK. This can be because
- there are concerns about the baby’s heart rate
- your baby is in an awkward position
- you’re too exhausted and have been pushing for a long time
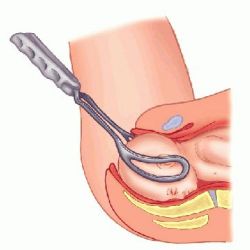
A forceps consists of two smooth metal long ‘salad spoon’ type instruments which are curved to shape around the sides of your baby’s head.
These are fitted carefully by the doctor and the handles of the forceps are then locked together securely. As you get a contraction the doctor will gently pull down onto the forceps as you push to guide your baby’s head to entrance of your vagina. When your baby’s head begins to crown and stretch your perineum the doctor may make a cut called an episiotomy to make the space in your vagina and perineum to allow for the baby’s head to be born. Once to the head is delivered the doctor will remove the forceps from around your baby’s head and wait for another contraction to deliver the shoulders and rest of your baby.
THINGS TO CONSIDER WHEN HAVING A FORCEPS DELIVERY:
- you are more likely to have an episiotomy which will require stitches which are done by the doctor (these are disolveable.)
- if you don’t have an epidural, local anaesthetic will be injected into the area before the doctor makes the cut so you not feel it
- you are more likely to bleed from the ‘cut’ (episiotomy) therefore your overall blood loss will be more
- if after 3 pulls the baby cannot be delivered in this way the delivery should be abandoned and a caesarean section should be considered
- therefore most forceps deliveries happen in theatre for this reason
- you should still be able to have skin to skin with your baby
- your can still have delayed cord clamping
- your birth partner can cut the cord
- you will require a catheter to be inserted into your urethra to empty your bladder of urine which usually stays in for 12 hours following the birth of your baby
- you have an increase chance of having short term incontinence problems such as not be able to control your wind or bowel movements
- you may feel more internal and external bruising from the forceps delivery than a ‘natural’ delivery
- you may therefore need stronger pain relief after the delivery to make you more comfortable especially when sitting to feed your baby or going to the toilet
- your baby is likely to be born with some markings on its face such as bruising on the side of the forehead and circular red marks around the cheeks. These should go after 24-48 hours
- due to bruising around your baby’ jaw and mouth they can find breastfeeding more difficult and you both may require extra support. Some women choose to use a Cranial Osteopath once discharged from hospital
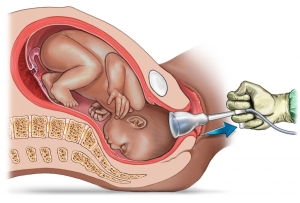
A ventouse delivery (or kiwi cup) is when a doctor applies a small silicone cup to the top of your baby’s head inside your vagina. Once the cup is in place, the air is sucked out of it using a foot-controlled vacuum pump, or a hand-held pump.
It can be noisy if a machine is used, so be prepared. When it is securely fixed, the doctor will ask you to push with your next contraction. The doctor will pull on the cup to help your baby out. Sometimes the cup comes off the baby’s head, which even if it sounds alarming, won’t cause any harm to your baby. After 3 pulls the baby’s head should begin to crown and stretch the perineum. Unlike a forceps birth where more space is require, with a ventouse delivery you are less likely to need an episiotomy. As the head is delivered the cup is removed so the doctor can deliver the rest of your baby.
THINGS TO CONSIDER WHEN HAVING A VENTOUSE DELIVERY:
- it can often be performed in the delivery room rather than theatre
- it is more likely to leave your baby with a temporary swelling on her head (cephalhaematoma).
- and more likely to cause bleeding inside your baby’s eye (retinal haemorrhage) which look like blood shot in the whites of your baby’s eyes
- you may not always need an episiotomy as less space is required of the instrument being used by the doctor
- you may still need a catheter inserted for up to 12 hours following the birth
- you should still be able to have skin to skin with your baby
- your should still be able to have delayed cord clamping
- your birth partner can still cut the cord
It is important to remember that if a doctor recommends an instrumental delivery you still have the choice to question their decision and where possible take time with your midwife and birth partner to discuss what is best for you and your baby. A good acronym to remember and to use at any point of your pregnancy or labour is BRAIN.
B – what are the benefits of doing what you recommend?
R – what are the risks?
A – what are the alternatives?
I – what does my intuition tell me?
N – what happens if we do nothing?
Sometimes it’s not always possible to avoid an assisted birth but good planning and preparation during your pregnancy can help you and your partner understand the options available to you. For example having an epidural increases your chance of having as assisted delivery because:
- It may slow your labour down, especially the second stage of labour when you have to start pushing, because it can be very difficult to know if you’re pushing correctly as you are numb in the area you need to focus on
- It increases the risk of your baby moving into the wrong position and therefore forceps or ventouse may be required to help turn the baby into a better position
But it’s equally important to weigh up the advantages and disadvantages. No one is going to think you’ve given up or couldn’t do it if you require an instrumental delivery. And the same goes for an epidural. Your birth is about it being positive for you and I have been at many many births where women had an epidural and a ventouse delivery and it’s been wonderful, beautiful and empowering. Milli Hill founder of The Positive Birth Movement says ” A good birth doesn’t have to be a hippy dippy ‘natural’ birth, all candles, knitting midwives and placenta smoothies. Many women who have hospital births that don’t go the way they planned and end in interventions such as an instrumental delivery, report feeling positive about what happened. Milli goes on to explain why, “This is because how a woman is spoken to and treated as she has her baby is much much more important than the actual mode of delivery. Women need to feel that they have been consulted, respected and given the information they need to make free choices in the best interest of themselves and their child. This allows them to begin motherhood feeling strong, capable and mentally healthy.”
And also please be reassured that eight out of 10 women who have an assisted birth have a normal birth next time around.
Has anyone else had an assisted delivery and would like to share their experience? Any tips on coping afterwards?
For more information about assisted deliveries please see: